3.1.1 The Continuum of Care Across the Lifecourse
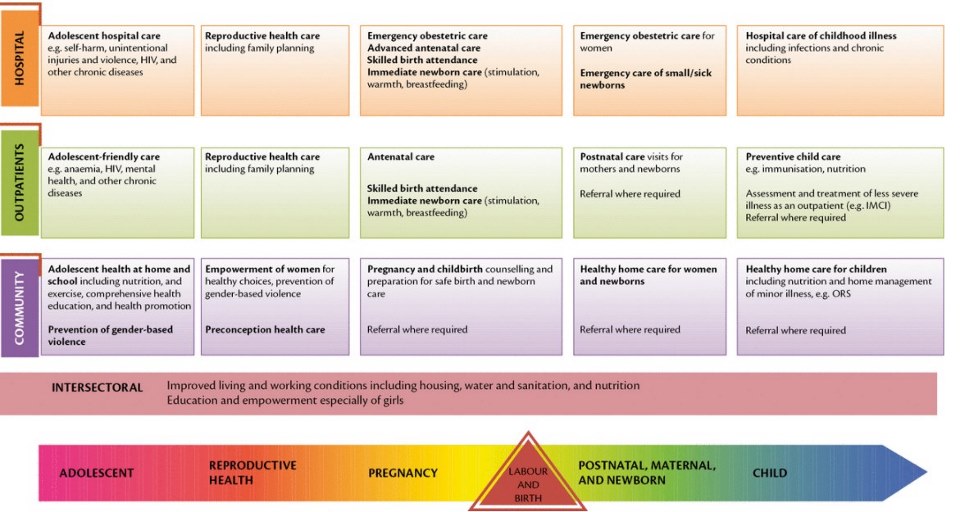
Neonatal services are part of a continuum of care that is comprised of two dimensions—the lifecourse and levels of care (Figure 3.1). This results in a matrix of integrated packages involving different types of care at different levels. More specifically, neonatal services are part of maternal and newborn care across a spectrum of SRMNCAHabbreviation services that begin before pregnancy and continue through labor and birth, the immediate postnatal period, the extended postnatal period, childhood and adolescence. Integrated service delivery extends from household to health facility and/or hospital and back home, along with a health system continuum of care.
The neonatal period merits special attention within humanitarian settings, when health services and systems may be interrupted and emergency support is brought in through national and international mechanisms. The newborn health services described in this Field Guide should be provided by governmental and non-governmental channels during a crisis response.
Although each humanitarian crisis presents different issues and challenges to responders, the life-saving interventions and commodities presented in this chapter have been defined according to WHOabbreviation approved standards for newborn care and, when systematically implemented, will improve MNHabbreviation outcomes in humanitarian settings. These recommendations should be adapted to local needs and used to improve guidelines already in place outlining minimum care and supply requirements for MNHabbreviation care in crisis and displaced settings.
Source: Lawn J, Sadoo S, Strategies through the lifecourse to improve maternal, newborn, child, and adolescent health, Oxford Textbook of Global Health of Women, Newborns, Children, and Adolescents, Oxford University Press, 2018.
3.1.2 Levels of Care
In humanitarian settings, staff working at all levels should deliver integrated maternal and newborn services across the continuum of care. This includes appropriate referral and follow-up across these three levels:
Hospitals and health facilities
These may include district, provincial, and national referral hospitals and temporary field hospitals. Inpatient referral care is provided by midwives, nurses and physicians with pharmacy and laboratory support services. Hospitals have the ability to provide more advanced MNHabbreviation care, such as CEmONC and advanced neonatal respiratory and feeding support.
Outpatient and outreach services
These facilities include existing host community primary care facilities, and other clinics operating out of permanent structures, which can be supplemented with temporary clinics in camp settings and mobile clinics. Some facilities at this level may be designated and equipped to deliver BEmONC services. Services are typically delivered by midlevel staff such as nurses and midwives, with support for referral to hospital if needed, and connections to community structures after discharge.
Family and community care
Evidence from low– and middle-income settings suggests dialogue and engagement of CHWs and men in promoting maternal and newborn health can improve care seeking behavior and home behaviors. Care at the household and community level is provided to women and babies in their homes or in camp settings by CHWabbreviation or other lay community members, TBAs, outreach workers or other trained health workers. These workers may be linked to a health post or primary care facility. The care is mainly promotive and preventive, with outreach.

