To ensure the safe, efficient transfer of newborns in humanitarian settings, use these simple tools:
- 4A: Job Aid: When to Refer a Newborn to the Hospital
- 4B: Job Aid: Transferring the Sick Newborn
- 4C: Sample Referral Note
Visit the Newborn Health in Humanitarian Settings Implementation Toolkit for more resources: www.healthynewbornnetwork.org.
6.4.1 Annex 4A: When to Refer a Newborn to the Hospital
For referrals from the household and primary health care (PHC) levels to the hospital.
Ask
- Is the baby having difficulty feeding?
- Has the baby had any convulsions (fits)?
Look, Listen, Feel
Count the breaths in one minute. Repeat the count if more than 60 breaths per minute.
- Look for severe chest indrawing.
- Measure axillary temperature.
- Look at the umbilicus. Is it red or draining pus?
- Look for skin pustules.
- Look at the young infant’s movements.
- If baby is sleeping, ask the mother to wake him/her. Does the baby move on his/her own?
- If the baby is not moving, gently stimulate him/her. Does the baby not move at all?
Refer when Any of the Following Signs are Present
- Not feeding well
- Convulsions
- Fast breathing (60 breaths per minute or more)
- Severe chest indrawing
- Fever (37.5°C[1] or above)
- Low body temperature (less than 35.5oC*)
- Movement only when stimulated or no movement at all
Action Before Transfer
- Give first dose of intramuscular antibiotics
- Treat to prevent low blood sugar (PHC level only)
- Advise mother how to keep baby warm on the way to the hospital
- Refer urgently
Ask
- How much does the baby weigh?
- How many weeks gestation was the pregnancy?
Refer when ANY of the Following Signs are Present
At household level:
- <2.5 kg
- <37 weeks gestation
At PHC level:
- <2.5 kg plus another severe classification
- <2.0 kg
Action Before Transfer
- Place baby immediately in KMCabbreviation position with mother or surrogate
- Refer urgently
Ask
Is the baby breathing normally, or is the baby gasping for breath?
Look, Listen, Feel
- Look at the baby and observe the breathing.
- Count the breaths in one minute.
- Look to see if the baby’s tongue is blue.
- Look to see if the baby is pale. Look at the tongue and palms.
- Feel the pulse and count the heart rate in 1 minute.
Refer when Any of the Following Signs are Present
First follow the Newborn Resuscitation Flowchart (Figure 3.2). Then refer if:
- Not breathing at all
- Gasping
- Respiration < 20 breaths per minute
- Heart rate < 100 per minute
- Tongue is blue
Action Before Transfer
- Advise mother how to keep baby warm on the way to the hospital
- Refer urgently
Ask
If jaundice is present, ask: when did the jaundice first appear?
Look, Listen, Feel
- Look for jaundice (yellow eyes or skin)
- Look at the baby’s palms and soles. Are they yellow?
Refer when Any of the Following Signs are Present
- Any jaundice if age less than 24 hours
- Yellow palms and soles at any age
Action Before Transfer
- Treat to prevent low blood sugar (PHC level only)
- Advise mother how to keep baby warm on the way to the hospital
- Refer urgently
Ask
Does the baby have diarrhea?[2]
Look, Listen, Feel
- Does the infant move on his/her own?
- Does the infant not move even when stimulated but then stops?
- Does the infant not move at all?
- Is the infant restless and irritable?
- Look for sunken eyes.
- Pinch the skin of the abdomen. Does it go back: Very slowly (longer than 2 seconds)? or slowly?
Refer when Two of the Following Signs are Present
- Movement only when stimulated or no movement at all
- Sunken eyes
- Skin pinch goes back very slowly
Action Before Transfer
- Advise mother how to keep baby warm on the way to the hospital
- Advise mother to continue breastfeeding
- Refer urgently
PHC Level Only
If infant has no other severe classification:
- Give fluid for severe dehydration
or If infant has another severe classification:
- Refer urgently to hospital with mother giving frequent sips of ORS on the way
- Advise mother to continue breastfeeding
6.4.2 Annex 4B: Job Aid: Transporting the Sick Newborn
Before transport
- Stabilize baby to the extent possible.
- Note that trained Community Health Workers (CHWs) can provide the initial dose of antibiotics, per protocol.
- Call receiving facility to notify them of the referral.
- Counsel family to explain why referral is necessary. Mother should accompany baby whenever possible.
- Fill out referral note (see Annex 4C for sample) and give to the caregiver or health worker accompanying the baby to the receiving facility.
- Record referred case in register.
On the way to the health facility
- If the baby is able to breastfeed, feed the baby at least every two hours. Give only breast milk.
- Keep the baby warm. Keeping the baby skin-to-skin is best. Ensure the baby is:
- Naked except for a nappy, hat and socks
- Placed between the mother’s breasts with the baby’s legs along her ribs and the head turned to the side
- Secured with a cloth
- If skin-to-skin care is not possible, wrap the baby well and keep her or him close to the mother.
- Where feasible, the health worker accompanying the caregiver and baby can provide counseling on care during transport, such as thermal care and breastfeeding.
After referral
- Where feasible, track counter-referral, including outcome of the referral and any follow-up actions required.
- Trained CHWs can undertake follow-up visits for referred newborns.
- Monitor and address barriers to the referral process.
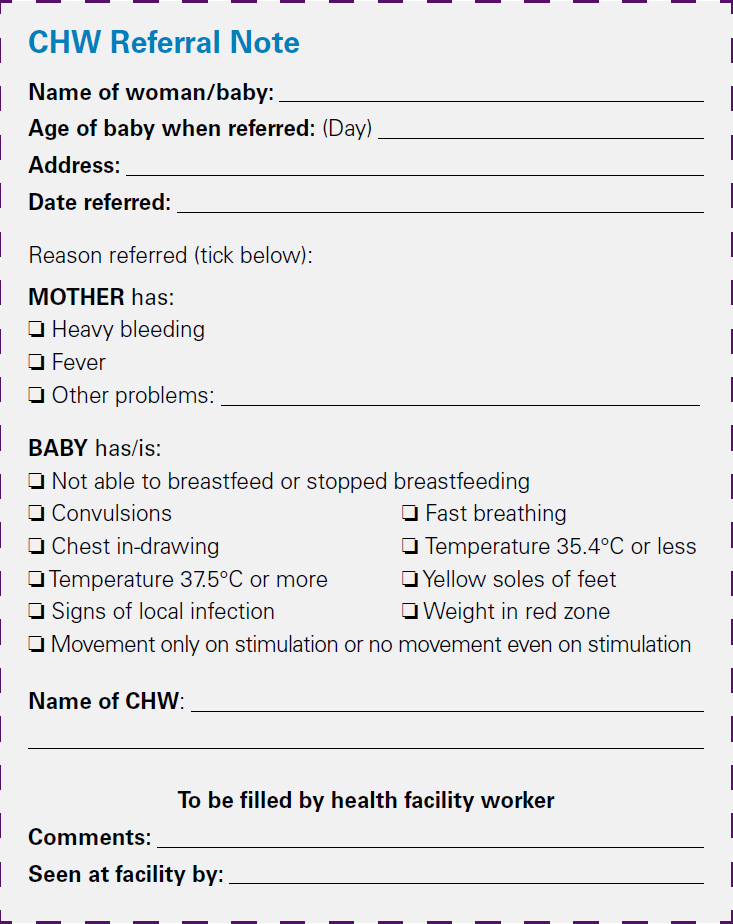
6.4.3 Annex 4C: Sample Referral Note
Note that pictorial referral slips can be developed in settings where community health workers are preliterate. See the Newborn Health in Humanitarian Settings Implementation Toolkit for samples: www.healthynewbornnetwork.org.